May 5, 2021:
This month, the Big Ten Cancer Research Consortium highlights our member, the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC). Get to know UMGCCC investigator Yixing Jiang, MD, PhD, and learn about a novel approach currently being tested to deliver treatment across the blood-brain barrier in high-grade gliomas.

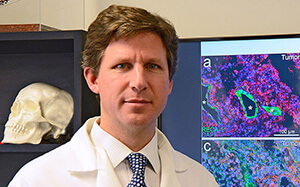
Yixing Jiang, MD, PhD
Associate Professor of Medicine; Director, GI Medical Oncology
University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center
Educational Background
- MD, Shanghai Medical College of Fudan University
- PhD, Mount Sinai School of Medicine
- Internal Medicine Residency: Mount Sinai School of Medicine
- Fellowship: University of Texas MD Anderson Cancer Center
Research and Clinical Interests
Dr. Jiang’s clinical expertise includes gastroesophageal, pancreatic, hepatobiliary and colorectal cancers. University of Maryland has the largest liver transplant center in Baltimore-DC area. Dr. Jiang is part of the multidisciplinary team managing patients with Hepatocellular Carcinoma referred to the center.
Dr. Jiang’s research interests are focused on:
- Drug development and early phase clinical trials. She has worked with NCI and industry in developing early-phase clinical trials. Recently, working with the biotechnology industry, she successfully completed first-in-human studies for a novel nanotechnology-based drug delivery system funded by the NCI. She collaborates closely with faculty from other institutions within University of Maryland system to develop and conduct trials using home-grown agents with federal funding support.
- Identification of predictive, prognostic markers and potential new therapeutic targets in gastrointestinal tumors by lipidomics. In collaboration with investigators at the University of Virginia, Dr. Jiang and her team utilized a mass spectrometry-based lipidomic approach to quantify sphingolipid changes in human pancreatic cancer tissue and plasma specimens from patients with pancreatic cancer.
- Chemotherapy-related peripheral neuropathy. Dr. Jiang is actively working with Kathleen Griffith, PhD, MPH, FNP-BC, on patient-based studies to develop preventive measures against chemotherapy-induced peripheral neuropathy. The study is funded by the NIH.
Little-known Facts
- Dr. Jiang enjoys cooking, hiking, and knitting.
Noninvasive Blood-Brain Barrier Disruption to Directly Deliver Chemotherapies to GlioblastomaD
The team that was first to offer a clinical trial in the United States opening the blood-brain barrier (BBB) with MRI-guided, focused ultrasound is now using the approach to direct chemotherapy into high-grade glioma tumors such as glioblastoma (GBM) and recurrent GBM (rGBM). Currently, two clinical trials at the University of Maryland Medical Center’s Brain Tumor Treatment and Research Center at the UM Marlene and Stewart Greenebaum Comprehensive Cancer Center (UMGCCC) are combining the strategy of using low-frequency (220 kHz) focused ultrasound and lipid-encased, gas-filled microbubbles to disrupt the BBB, allowing for the penetration of chemotherapeutic agents into tumor-infiltrated brain tissues. The portfolio of clinical trials at the University of Maryland now also includes a newly opened trial for rGBM exploring the use of carboplatin – a chemotherapy that might demonstrate improved efficacy against malignant brain tumor cells once the BBB is overcome.
“We are pleased to be among the first in the world to be exploring ways of treating GBM that were impossible before recent advances in focused ultrasound,” says Graeme F. Woodworth, MD, FACS, Professor and Chair of the Department of Neurosurgery at the University of Maryland School of Medicine and director of the Brain Tumor Treatment and Research Center at UMGCCC. “Blood brain barrier disruption is a major opportunity for treating numerous neurological conditions, including Parkinson’s disease and Alzheimer’s disease,” he continues. “However, as this treatment strategy has the potential to improve drug treatment and survival for patients with aggressive brain tumors, applying it to that end is one of our top priorities.”
GBM is thought to have a poor prognosis in large part because of the diffuse way glioma cells invade healthy brain tissue. Even after primary tumor resection, traces of GBM remain at the margins of the tumor bed, unable to be removed safely and not even visible on contrast-enhanced MRI. The standard of care for primary GBM includes a six-week course of concurrent radiotherapy and chemotherapy in the form of oral temozolomide (TMZ) followed by an adjuvant course of TMZ one week a month for six months. However, even after TMZ was added to this protocol – which increased median survival from 9–12 months to 14.6 months – recurrence is inevitable, and 5-year survival rates for GBM are less than 5 percent.
To potentially find better treatments for GBM, it is anticipated that the two trials will provide evidence that serial temporary blood-brain barrier disruption (BBBD), through the use of low-frequency focused ultrasound and the stable oscillation of circulating microbubbles, is a safe and feasible way to administer localized chemotherapy drugs in the residual tumor-invaded brain regions or in the setting of recurrent GBM tumors.
The BBB protects the brain from neurotoxins and viral infections through tightly connected, specialized endothelial cells supported by a complex network of astrocytes, pericytes and microglia; without intervention, this protective quality also makes it impenetrable to all but small lipophilic molecules, severely limiting therapeutic options.
Woodworth and others from the University of Maryland and Mayo Clinic Arizona have reviewed the various strategies for opening the BBB to treat GBM more directly,1 perhaps with lower, safer chemotherapeutic doses. In an application that UM researchers described in a 2016 paper, microbubbles can mechanically disrupt the blood-brain barrier when augmented with focused ultrasound.2 The team believes this is a particularly promising approach for the following reasons:
- Noninvasive – The technology is applied transcranially.
- Safe – Gas-filled microbubbles allow for focused ultrasound sonication efficacy at a lower frequency that does not heat tissues and cause treatment-related side effects.
- Temporary – After the application of focused ultrasound with microbubbles, the BBB remains open for 4–6 hours before closing again.
- Targetable – BBBD can be limited to the regions of the brain near the tumor.
- Closed Feedback Loop Control – The focused ultrasound treatments are monitored and controlled in real-time via acoustic emission monitoring systems.
BBBD is achieved through harnessing the Exablate 4000 Type 2.0/2.1 transcranial focused ultrasound technology (Insightec) and intravenous contrast DEFINITY® microbubbles (Lantheus Medical Imaging). Sonication by the ultrasound transducer produces acoustical, non-inertial cavitation of the 1–5 m microbubbles in the blood-brain barrier capillaries, temporarily opening the junctions between the endothelial cells in the BBB.
1Harder BG, Blomquist MR, Wang J, Kim AJ, et al. Developments in blood-brain barrier penetrance and drug repurposing for improved treatment of glioblastoma. Front Oncol. 2018;8:462. doi: 10.3389/fonc.2018.00462
2Hersch DS, Kim AJ, Winkles JA, Eisenberg HM, et al. Emerging applications of therapeutic ultrasound in neuro-oncology: moving beyond tumor ablation. Neurosurgery. 2016;79(5):643-654. Doi: 10.1227/NEU.0000000000001339
About the Big Ten Cancer Research Consortium: The Big Ten Cancer Research Consortium was created in 2013 to transform the conduct of cancer research through collaborative, hypothesis-driven, highly translational oncology trials that leverage the scientific and clinical expertise of Big Ten universities. The goal of the Big Ten Cancer Research Consortium is to create a unique team-research culture to drive science rapidly from ideas to new approaches to cancer treatment. Within this innovative environment, today’s research leaders collaborate with and mentor the research leaders of tomorrow with the unified goal of improving the lives of all patients with cancer.
About the Big Ten Conference: The Big Ten Conference is an association of world-class universities whose member institutions share a common mission of research, graduate, professional and undergraduate teaching and public service. Founded in 1896, the Big Ten has sustained a comprehensive set of shared practices and policies that enforce the priority of academics in the lives of students competing in intercollegiate athletics and emphasize the values of integrity, fairness and competitiveness. The broad-based programs of the 14 Big Ten institutions will provide over $200 million in direct financial support to more than 9,800 students for more than 11,000 participation opportunities on 350 teams in 42 different sports. The Big Ten sponsors 28 official conference sports, 14 for men and 14 for women, including the addition of men’s ice hockey and men’s and women’s lacrosse since 2013. For more information, visit www.bigten.org.
















Subscribe to the Big Ten CRC Newsletter X
X Facebook
Facebook YouTube
YouTube